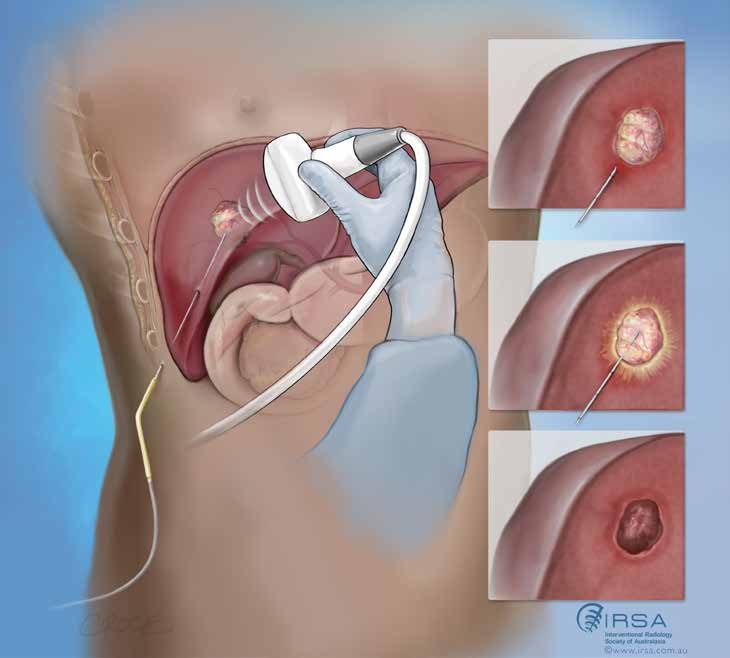
WHAT IS IMAGE GUIDED TUMOUR ABLATION?
Tumour ablation is the process whereby a needle is placed directly into a tumour and a treatment is delivered aiming to kill the tumour in place. This can be achieved through a variety of ways but the most common is via heating or cooling the tumour. Other approaches that can also be used in difficult tumour locations include injection of a chemical (usually alcohol or acetic acid) or use of electricity passed through the cells.
WHY WOULD MY DOCTOR REFER ME TO HAVE THIS PROCEDURE?
If you have been diagnosed as having a tumour, image guided tumour ablation is used as an alternative to surgery with curative intent if surgery is felt to be too high risk or for palliation (improving quality of life or length of life, but not destroying all tumours).
Occasionally, ablation may be the best treatment due to it being less invasive than surgery with similar efficacy, such as in some benign tumours of the bone or in small primary liver cancers.
Wondering If You Qualify for IMAGE GUIDED TUMOUR ABLATION?
How do I prepare for the procedure?
The need for having a procedure to destroy or reduce a tumour is usually assessed using ultrasound, CT scan or MRI, and sometimes all three. These imaging tests will be used to determine the size, location and other features of the tumour as a guide for planning the procedure. The test will also be used in future assessment of the response to treatment. Please bring all available scans you have to any appointment or procedures.
Blood tests will also be carried out to ensure there are no medical reasons why ablation should not be used, and tumour marker blood test results may also be used to assess your response to the ablation. Fasting (no food or fluid) is usually required for 6 hours before the procedure.
You will generally be admitted to hospital or to a day procedure centre on the day of the procedure if you are not already in hospital. Ablation can be carried out under general anaesthetic where you will be asleep and monitored by an anaesthetist (specialist doctor). Alternatively, ablation can be done under deep sedation but without a full anaesthetic; this can be done if full general anaesthesia is risky for you.
What happens during the procedure
After you have received the anaesthetic, you will be positioned to allow the interventional radiologist with access to the target tumour and images will be taken to target the treatment.
The area where the needle electrode will be inserted is cleaned with antiseptic solution and covered with a surgical drape. The area will be numbed with a local anaesthetic. A very small cut is made in the skin after it is numb and then the ablation needle electrode(s) are inserted into the tumour being treated using imaging guidance, and images or pictures are shown on a screen. Once the electrode is confirmed to be in the desired position at the tumour, the treatment is applied.
At the end of the procedure, the needle(s) will be removed, and pressure will be applied to the site where the needle was inserted. The opening in the skin is covered with a dressing and is normally too small to need a stitch.

What is the recovery
normally like?
For most patients’ recovery from ablation is relatively fast, and you can normally walk and eat the night of the procedure and go home the next day. You should refrain from any heavy lifting or strenuous activity for the rest of the week you are treated.
Pain: It is common to have some discomfort following your procedure. This can last a few days and is usually mild.
Flu-like symptoms: Approximately one in four patients may develop flu-like symptoms, but this is not due to having the flu, which is the result of infection with influenza virus. The flu-like symptoms, such as a slight fever and loss of energy, usually last for less than 5 days and can be treated with paracetamol.
The use of CT scan to guide the procedure involves x-rays: While there is a slight increase in the risk of cancer from any kind of radiation exposure, it is considered that the benefits outweigh this very small risk in most cases of tumour ablations.
Bleeding: Bleeding is the most common major complication from ablation. The risk of bleeding is low at less than 2% of people receiving the treatment. This will depend exactly on where your tumour is and will be discussed with you prior to the procedure being carried out.
Infection: As a small cut is made in the skin during the procedure, there is a small risk of infection. The chance of infection requiring antibiotic treatment is less than one in 1000 people who have this treatment.
Burns: Burns in the skin covered by the grounding pads may occur, but this happens in less than two in 1000 people who have the treatment.
Damage to adjacent organs: These include damaging the bowel, bile duct and lung tissue in radiofrequency ablation of cancer
in the liver, but the risk is small, less than two in 1000 people having the treatment. The use of imaging guidance is intended to minimise this risk.During ablation of the kidney, the ureter (the tube connecting the kidney to bladder) may be injured in less than two in 100 people who have the procedure.
When ablation of the lung is carried out, air inside the chest cavity causing collapse of the lung occurs in one in every two cases, but only one in five cases needs treatment. The treatment involves putting a tube into your chest to drain the air. Fluid may also collect between the lung and the chest wall in less than one in five cases, but this usually does not require any treatment and, generally, you would not notice it if the amount of fluid is small (which is usually the case).
With radiofrequency ablation of bone cancer or a non-cancerous bone mass, cases of fracture or injury to the surrounding nerve, skin and muscles have rarely been reported.
What are the benefits?
Ablation is less invasive than surgery and can offer a curative or palliative benefit like surgery in correctly selected cases.
As no surgical incision is required, it takes less time to recover and discomfort is usually minimal.
Because a larger amount of normal tissue is spared using ablation, the function of the involved organ, such as liver, kidney, and lung, is better preserved. This benefit is a trade off in terms of the chance of the tumour recurring. This may be higher than or similar to the chance of recurrence after surgery. Ask your specialist for the expected chance of success of the procedure in controlling your tumour as this differs depending on the type, size, and location of tumour/s.
HOW LONG DOES IT TAKE TO RESPOND TO THE PROCEDURE?
The cells in the tumour should die immediately after the ablation. You should feel back to normal within two weeks of the procedure.
Follow up will be needed. The exact extent of cells killed during the procedure may be obscured by inflammation, a natural body reaction to the procedure. The inflammation will gradually decrease in 1 or 2 weeks. A CT scan, or less commonly an MRI scan, will be taken approximately 1 month after your treatment to assess the results of the procedure.
It is important to realise that a period of follow up is required after ablation. It often takes a year (sometimes longer) to be certain that the tumour is treated. This requires both imaging and visits to your specialist doctor.
Find a Doctor
Our Doctor Finder is a comprehensive database of interventional radiologists practicing in Australasia.
Use the search fields to search based on geographic location or by area of practice.
